Preschool-aged children in early-stage type 1 diabetes have changes in blood sugar levels, even before they are officially diagnosed
New research has found that preschoolers who are in the early, pre-symptomatic stages of type 1 diabetes (T1D) have changes in blood sugar levels well before symptoms appear.
We used to think that people developed T1D when they first showed the ‘4T’ symptoms: thirst, tiredness, toilet (increased urination) and thin (weight loss). This is when T1D is typically diagnosed, and when insulin therapy starts. However, years of research have changed our understanding of the condition, and we now know T1D starts months or even years before these symptoms develop.
Most people at this stage do not know they are in the early stages of the condition, called ‘early-stage’ or ‘presymptomatic’ T1D.
Read more about the stages of T1D and why they’re important here.
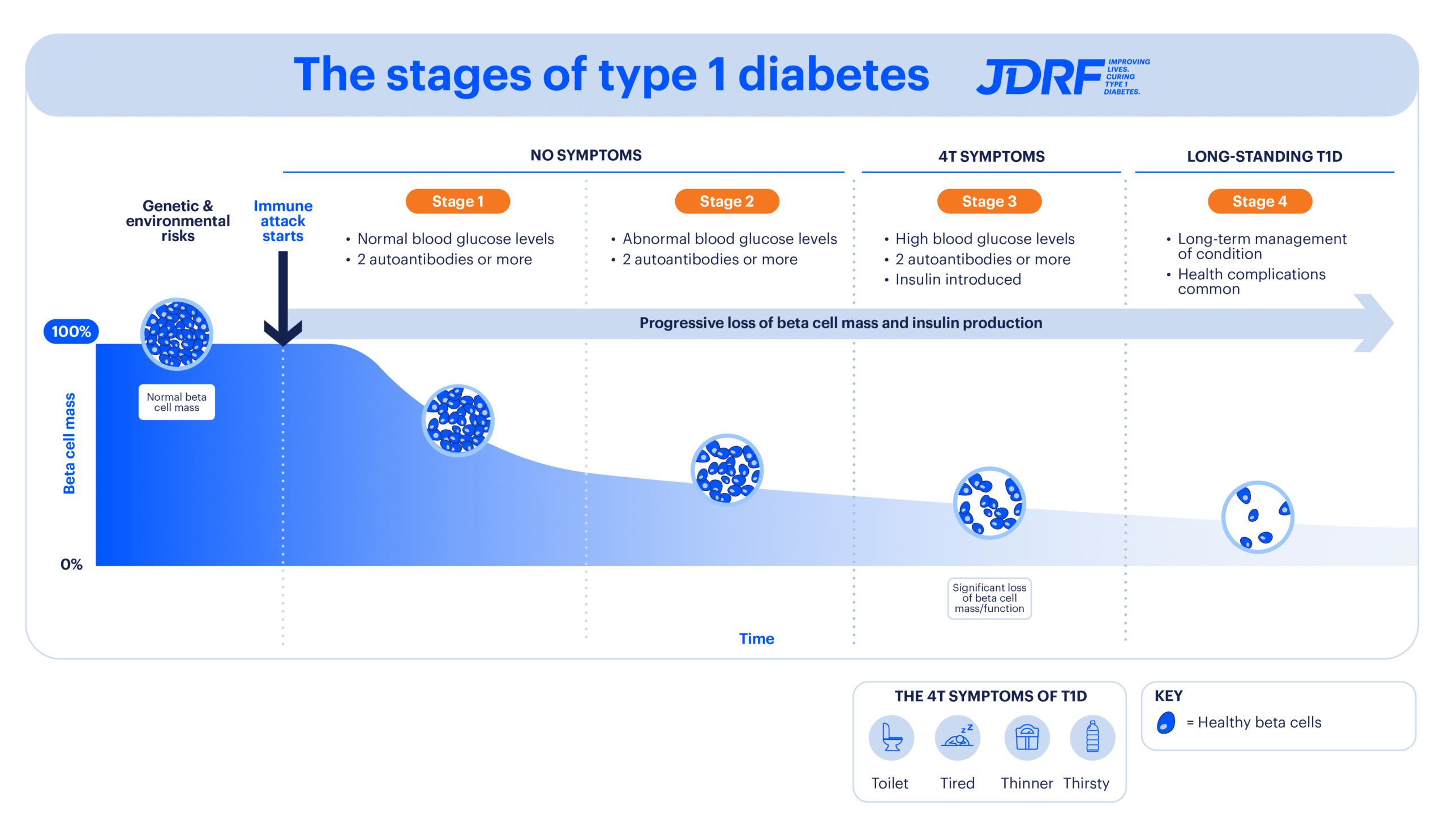
There are several stages of T1D development, which progress over time. In those who are genetically susceptible, environmental triggers start the body’s immune attack on insulin-producing beta cells. Two or more autoantibodies can be detected in the blood from as early as Stage 1 T1D, and blood sugar levels become more difficult to control as the condition progresses. Stage 3 is when T1D is normally diagnosed with the development of the 4T symptoms. Stage 1 and 2 are called early-stage or presymptomatic T1D. Stage 3 is called symptomatic T1D.
To better understand these early stages, researchers from the Environmental Determinants of Islet Autoimmunity (ENDIA) study measured the blood sugar levels of preschool-aged children who had persistent islet autoantibodies, a marker of early-stage T1D. This is the first time sugar levels have been measured in such young children using continuous glucose monitoring (CGM). The study, led by Dr Aveni Haynes from The Kids Research Institute Australia, The University of Western Australia, has recently published its findings in the journal Diabetes Care.
ENDIA is jointly funded through JDRF Australia and the Leona M. and Harry B. Helmsley Charitable Trust (Helmsley). The ENDIA CGM study was supported by grants from Diabetes Research Western Australia, the Women and Children’s Hospital Research Foundation, the Australasian Paediatric Endocrinology Group, and the Helmsley (grant key 2205- 05241).
What did the research investigate?
The researchers used CGM devices on 31 children with early-stage T1D and compared their blood sugar levels with 24 children of a similar age without the condition. The children used CGM devices for a minimum of 14 consecutive days. The CGM devices were ‘blinded’ which means neither the children nor their parents could see the CGM results.
CGM was used as it is a less invasive way of measuring blood sugar levels compared to having blood tests in these young children and records sugar levels every 5 minutes, 24 hours a day for up to 10 days in a row.
What did the study find?
The study found that the children with early-stage T1D had more variability in their sugar levels and spent less time in the ‘target’ healthy range. People without T1D spend most their time in this range. The children with early-stage T1D also spent more time at higher blood sugar levels compared to those without early-stage T1D.
What does this mean for the T1D community?
This study provides new information showing that changes in sugar levels can be identified using CGM in very young children with early-stage T1D, even before overt symptoms are present. The study also adds to research efforts underway that are investigating whether sugar levels and patterns measured using CGM could be used to predict the risk of developing symptomatic T1D, as well as its use in identifying and monitoring which stage of T1D an individual is in.
Further work is being undertaken by the research team to investigate how and when blood sugar levels change in children with early-stage T1D. This information is key to developing strategies to delay, and ultimately prevent symptomatic T1D.
How was JDRF involved?
JDRF Australia has been a long-term supporter of the ENDIA study, which seeks to understand how genetic susceptibility and environmental factors combine to initiate and progress T1D development in individuals. It is the world’s first study tracking T1D development from as early as pregnancy through to childhood.

Dr Aveni Haynes, lead of the study
Dr Haynes has also received a JDRF Career Development Award (CDA), a highly competitive and internationally prestigious award that supports up-and-coming research leaders in the field of T1D, allowing them to focus on research that aligns with JDRF’s strategic goals and priorities.
Our research portfolio
Ground-breaking projects like these are only possible with support from our community. The future of 130,000 Australians living with T1D and the 8 more diagnosed each day depends on it.
To get involved, donate here.
Explore all research projects that JDRF Australia funds.