Complications and impacts of type 1 diabetes
Go to specific articles on: Eye problems | Gum disease | Heart and blood vessels | Kidney damage (nephropathy) | Nerve damage (neuropathy)
Type 1 diabetes complications
As most people who live with type 1 diabetes (and their loved ones) know, the condition isn’t the kind of thing you can ignore. There are no days off. And if you drop the ball on managing your condition, you can end up with short or long-term complications that can significantly impact your life.
It’s sobering stuff, but when you’re living with type 1 diabetes (T1D), knowledge is power. With that in mind, it’s important to know that when compared to the general population, people living with T1D have a higher chance of:
- developing eye damage
- developing nervous system damage
- developing kidney disease
- being diagnosed with a second autoimmune disease.
But it’s not all bad news, as there are things you can do to reduce your chance of developing complications. Find out more about the potential health impacts so you can look after yourself for longer.
Short-term complications of type 1 diabetes
Short-term complications of type 1 diabetes are usually related to your blood glucose levels (BGLs) falling out of the targeted range your healthcare team has set for you. These include hypoglycemia, hyperglycemia and diabetic ketoacidosis (DKA).
Hypoglycemia
Managing your blood glucose levels on a daily basis can be a delicate balancing act. Ultimately, you’re trying to avoid hypoglycemia (or a ‘hypo’), which means abnormally low blood glucose levels.
Hypo symptoms include:
- shakiness
- sweating
- light-headedness
- weakness
- blurred vision
- irritability
- in extreme cases, seizure or loss of consciousness.
Hypos can occur if you take too much insulin, if you delay or skip a meal, or drink alcohol without eating. You could also trigger a hypo if you do intense exercise and fail to adjust your food or insulin intake.
Regular hypos can impact your quality of life and your memory or focus. It may even lead to hypoglycemia unawareness, where your body becomes less sensitive to the warning signs of a hypo. So it’s worth taking the time to ensure your BGLs are in targeted ranges as much as possible.
Hyperglycaemia
Hyperglycaemia is the opposite to hypoglycemia: it happens when your blood glucose levels are too high and there’s not enough insulin in your body to bring down your BGLs.
Insulin acts a bit like a key, enabling the sugar in your blood to enter your cells and be used for energy. But if that isn’t happening, the sugar stays in your bloodstream and causes hyperglycaemia.
It’s normal to have hyperglycaemia when you’re living with type 1 diabetes, and it’s something that’s usually managed with insulin. But if your body doesn’t have insulin for around eight hours, things can become dangerous.
Diabetic ketoacidosis
Diabetic ketoacidosis (DKA) is a serious condition. For some people, the symptoms of DKA can be the first obvious sign that they have type 1 diabetes.
DKA occurs because your body can’t produce insulin, and if your blood glucose rises without enough insulin on board to bring your levels back to normal, your body starts to break down fat as fuel. This leads to a build-up of ketones (or acids) in your bloodstream. Untreated, this can lead to diabetic ketoacidosis.
Along with high BGLs and high ketone levels in your urine, the warning signs of DKA can include:
- being very thirsty
- needing to urinate a lot
- stomach pain
- nausea or vomiting
- feeling weak
- feeling confused
- having fruity-smelling breath.
If you’re experiencing any of these, seek medical help immediately.
Long-term complications of type 1 diabetes
Living with type 1 diabetes can lead to long-term complications that add up over time – especially if BGLs aren’t controlled well. Common conditions include vision problems, nerve issues, kidney disease and other issues.
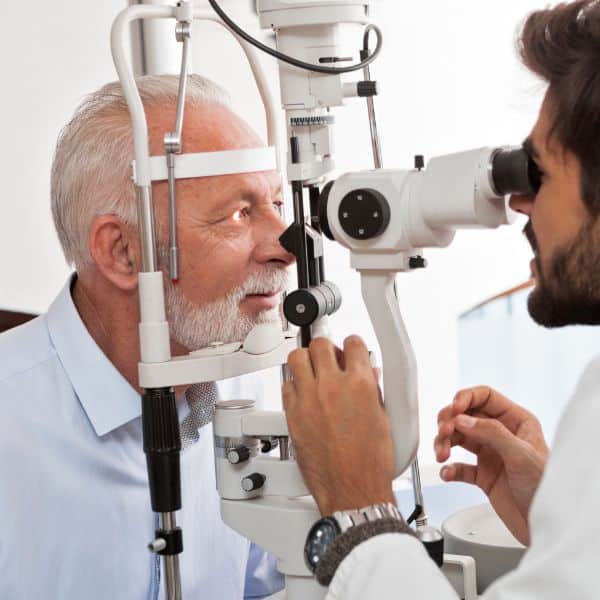
Diabetic retinopathy and eye problems
In the short term, high BGLs can lead to blurred vision. This should return to normal once you get your glucose levels stable again.
But over time, high BGLs can lead to more serious eye problems, such as diabetic retinopathy. Around one in three people with diabetes have some form of this condition. It happens because the tiny blood vessels of the retina, at the back of the eye, get damaged.
If you don’t treat diabetic retinopathy, it can lead to vision loss.
Other long-term impacts of T1D include diabetic macular oedema. People living with T1D are also two to five times more likely to develop cataracts than the general population.
Read more about eye problems in people with T1D.
Diabetic neuropathy
Consistently high BGLs can lead to nerve damage, known as diabetic neuropathy. This happens when nerves stop sending messages to different parts of your body, resulting in anything from mild numbness (usually in the legs or feet) to significant discomfort or pain.
Up to 50% of people with diabetes suffer from diabetic neuropathy.
Diabetic neuropathy develops slowly. If you start to notice symptoms, early diagnosis and treatment can stop it getting worse.
Look out for:
- pain or numbness in your arms or legs, especially at night
- not being able to feel cuts or sores
- having problems walking
- not being able to spot when your BGL is low
- having heat intolerance.
Read more about diabetic neuropathy.
Kidney disease
Your kidneys play a major role in filtering waste and excess fluid from the blood. Kidney disease (or kidney nephropathy) is a common complication of T1D.
Nearly one in three people with T1D develop kidney disease, but most don’t end up with kidney failure.
Kidney disease can happen because high levels of sugar in the blood can damage the tiny ‘filtering’ units in the kidneys, forcing them to work harder. Once your kidneys are damaged, they can’t filter blood like they should, so wastes build up in the body.
There’s no cure for kidney disease, but early treatment can help prevent further damage.
Risks associated with type 1 diabetes
While type 1 diabetes can lead to a number of complications, it can also increase your risks of other conditions, as well. For example, compared to the general public, people with T1D have a two to 10 times higher risk of cardiovascular disease
You can also experience a higher risk of complications with pregnancy. Complications can include miscarriage, abnormal development in your baby and pre-eclampsia. Working closely with your healthcare team can help minimise these risks, and the majority of women who live with diabetes go on to have healthy babies.
Preventing complications
Although type 1 diabetes can have its challenges, there are ways to avoid complications and the more significant risks it may pose to your health.
- Monitor your blood glucose levels regularly. No matter the system you use to check your BGLs, it’s important to manage your levels and stay in the target range.
- Never miss a medical check-up. That includes regular eye screenings, and getting your blood pressure, cholesterol and kidneys checked at least once a year.
- Stay educated. Reading up about type 1 diabetes and new treatments or research can help you stay one step ahead of your condition.
- Review your treatment plan. Things change in your life, so it’s important to talk to your healthcare team and review your diabetes management plan a few times per year.
Type 1 diabetes can increase your chance of other health problems and developing complications that can have an impact on your life. But with the right education, treatment and diabetes management, people living with T1D can live long and satisfying lives.
Sources
- Cardiovascular disease in patients with type 1 diabetes: Early evaluation, risk factors and possible relation with cardiac autoimmunity (Diabetes Metabolism Research and Reviews)
- Deaths among people with diabetes in Australia (Australian Institute of Health and Welfare)
- Diabetes and kidney failure (Better Health Channel)
- Diabetic neuropathy (Better Health Channel)
- Diabetic neuropathy (Health Direct)
- Diabetic neuropathy (Mayo Clinic)
- Diabetic retinopathy (National Eye Institute)
- Diabetic retinopathy (The International Agency for the Prevention of Blindness)
- Excess cardiovascular risk in type 1 diabetes mellitus (Circulation)
- Hypoglycaemia (Diabetes SA)
- Hypoglycaemia unawareness (Diabetes Australia)
- Life expectancy of type 1 diabetic patients during 1997–2010: a national Australian registry-based cohort study (Diabetologia)
- Pregnancy when you have diabetes (Diabetes Australia)

I am interested in hearing more about…
