Regenerating damaged beta cells in type 1 diabetes: new funding announced
JDRF has funded a new Australian research project which may allow those with type 1 diabetes (T1D) to regenerate lost pancreatic cells.
During T1D development, the immune system mistakenly attacks the insulin-producing beta cells in the pancreas. This leads to the loss and destruction of beta cells, meaning that people with T1D are no longer able to make their own insulin, a hormone crucial for controlling blood glucose levels.
To meet our mission of a world without T1D, JDRF has announced funding of $1.1 million to a project led by Professor Sam El-Osta from the Baker Heart and Diabetes Institute, which will investigate whether new beta cells can be regenerated from pancreatic tissue in those with T1D.
The promise of a cure for T1D
Replacing destroyed beta cells from sources outside the body or regenerating beta cells from within the body holds promise for a cure for T1D.
It has been shown that islet transplantation and whole pancreas replacement using donor tissues or organs reduces or removes the need for injecting insulin in those with T1D. However, the limited availability of donors, along with the need for life-long immunosuppression, make this option unsuitable for the majority of people living with T1D.
As part of JDRF’s research strategy around the world, we are funding projects focusing on alternative and innovative sources of beta cells, and ways to transplant them into the body to allow people with T1D to make their own insulin again. This includes the regeneration of beta cells from a person’s own tissues.
What the project will focus on
Previous breakthrough studies from Professor El-Osta’s lab showed that FDA approved drugs known as EZH2 inhibitors can stimulate the growth of new beta-like cells from a person’s own pancreatic tissue. These cells were able to respond to glucose and produce insulin, an important sign that they may be able to replace lost beta cells in those with T1D.
This suggests that someday people with T1D may be able to reverse the condition following administration of such drugs.
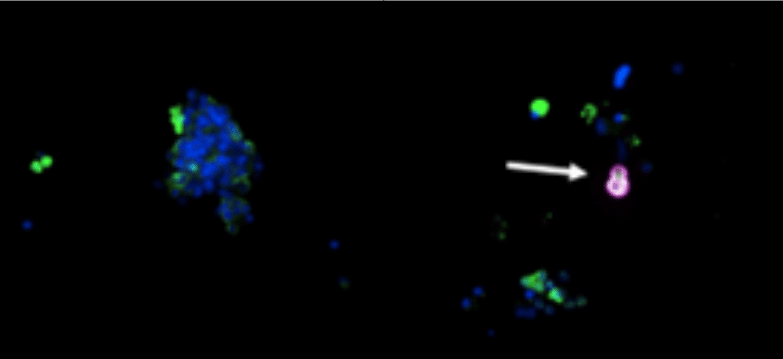
Image: How EZH2 inhibitors can induce the production of insulin in those with T1D. Left image shows the pancreas of someone with T1D. The right image shows a T1D pancreas treated with an EZH2 inhibitor which can now produce insulin (pink colour and arrow).
However, these findings were proof-of-concept investigations, meaning much more research is needed to determine whether these treatments hold a key to curing T1D. Thus, the current funding will extend the work to pre-clinical models to see if these drugs are able to restore insulin production from newly formed beta cells and reduce high blood glucose levels (hyperglycaemia).
If successful, this approach could offer a promising new treatment for T1D, addressing the current limitations of pancreatic donor shortages and side effects from other treatments like islet transplantation. Importantly, as some of the drugs used in regenerating beta cells are already approved in the United States for the treatment of certain cancers, regulatory approval for their use in T1D may be fast-tracked.

“Using pancreatic cells derived from T1D donors we’ve shown regenerative capacity in the pancreas despite absolute beta cell destruction. While these were important findings, more work is needed to rapidly translate this research to people living with T1D. This JDRF funding will allow us to advance this research to the next stage and has the potential to become a disease-modifying therapy. We are focussed on regenerating insulin producing beta cells by harnessing the patient’s pancreatic cells for the treatment of diabetes.”
Professor Sam El-Osta
About this research
Professor El-Osta’s research project is funded by JDRF International Grant # 2-SRA-2024-1442-S-B.
Our research portfolio
Groundbreaking projects like these are only possible with support from our community. The future of 130,000 Australians living with T1D and the 8 more diagnosed each day depends on it.
To get involved, donate here.
Explore all research projects funded by JDRF Australia.