New research funding may allow those with type 1 diabetes to make insulin again

JDRF has just funded a new Australian islet transplantation research project with the potential to revert type 1 diabetes.
The benefits of islet transplantation
Pancreatic islet transplantation is a life-saving and life-changing treatment currently available for people with type 1 diabetes (T1D) who are unaware of their dangerously low blood glucose levels (known as ‘severe hypoglycaemia unawareness’).
T1D occurs when the body’s own immune system mistakenly attacks the insulin-producing beta cells within structures called islets of the pancreas. As a result, people with T1D lose the ability to produce insulin to regulate their blood glucose levels and need to replace this insulin through daily injections or automated insulin delivery systems for the rest of their life.
Islet transplantation involves the isolation of healthy islets from an organ donor and their transplantation into someone with T1D. This prevents the person from experiencing severe hypoglycaemia and allows them to produce their own insulin once more, reducing the amount of injected insulin they need. It also allows natural control of blood glucose levels, which has significant benefits in reducing long-term health complications associated with T1D, such as kidney disease, vision loss and cardiovascular disease.
Why islet transplantation is not yet an option for all
Despite the benefits of islet transplantation, there remain significant challenges.
Firstly, is the limited availability of organ donors and the difficulty of isolating the islet cells, which makes the supply of healthy islets a substantial barrier. Secondly, just like other organ donations, there is the need to take life-long immunosuppressive drugs which not only have toxic effects on the body but can also increase the risk of infections and health issues including the potential development of various cancers. This means that currently islet transplantation is only provided to a limited number of Australians with T1D.
To achieve our vision of a world without T1D, JDRF prioritises research to find cures for the condition, including research which focuses on novel sources of pancreatic islets and beta cells for transplantation. As a result, JDRF has announced $3.5 million of funding for a project led by Professor Wayne Hawthorne at the University of Sydney and the Westmead Institute for Medical Research.
This project is investigating how alternative sources of pancreatic islets — specifically from genetically modified pigs — could solve the shortage of human islets and reduce the need for immunosuppressants. If it is successful, this could mean more Australians with T1D would be able to access this life-saving technology.
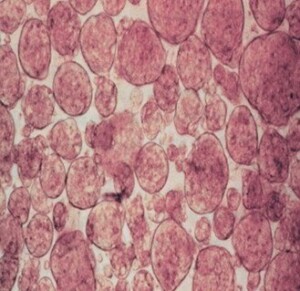
Image: Islet-like cell clusters as novel sources of pancreatic beta cells. Image courtesy of Professor Wayne Hawthrone
New project is researching ways to improve islet transplantation
Xenotransplantation is the transplantation of animal tissues, cells, or organs into human recipients. Advances in the past decade have meant that we are now moving into clinical studies investigating the use of genetically modified pig hearts and kidneys in humans for a range of conditions.
However, xenotransplantation for T1D is still in its early stages, as pig islets provoke a powerful immune response once transplanted into humans, meaning that the transplants are not likely to survive the host’s immune attack.
The aim of the recently funded project, led by Professor Hawthorne, is to find new ways to circumvent the human immune response, using genetically modified pig islets to be transplanted into those with T1D.
The project will use a pre-clinical model to test whether altering the genes in the donor pig is able to reduce the post-transplantation immune response, so that immunosuppressive drugs are not required, and the islets are not rejected. This would potentially be able to provide an infinite source of islets. This would be a gamechanger for those with T1D and bring us one step closer to reversing T1D.
Australia stands as a global frontrunner in islet xenotransplantation, and Professor Hawthorne and his team have played a significant role in placing us on the international map. For example, Professor Hawthorne has been elected the President of the International Xenotransplantation Association (IXA). The funded project is a long-standing collaboration with other teams around Australia including Professors Peter Cowan (St Vincent’s Hospital, University of Melbourne) and Mark Nottle (University of Adelaide). Together, they have been working to find a cure for T1D for over 25 years.

“Our ultimate goal is to establish xenotransplantation as a safe and effective treatment option for all individuals with T1D, not just a select few. We hope that our research will allow those with T1D to make insulin once again, safely, and without the need for life-long immunosuppression.”
Professor Hawthorne, Director of the National Pancreas and Islet Transplant Laboratories, Westmead Hospital and Director of the Xenotransplant Research Program, Westmead Institute for Medical Research.
About this research
Professor Hawthorne’s research project is funded by JDRF International Grant #3-SRA-2023-1418-S-B.
Our research portfolio
Groundbreaking projects like these are only possible with support from our community. The future of 130,000 Australians living with T1D and the 8 more diagnosed each day depends on it.
To get involved, donate here.
Explore all research projects that JDRF Australia funds.