Five Innovative New Research Projects Funded

JDRF is excited to announce more than $2.7 million in funding to kick start five highly innovative research projects.
The 2021 Pilot and Innovation Awards are designed to support innovative new directions for type 1 diabetes research, including concepts that have never been investigated before. The focus is on early-stage work that has a large potential to change the way we diagnose, treat and manage T1D.
This year’s recipients are exploring new frontiers in genomics, islet transplantation, immune therapies and drug delivery to expand the horizons of T1D research.
This year’s Pilot and Innovation Award recipients are:

Prof Simon Barry, University of Adelaide
Using genomics to uncover the components of T1D risk
While we know that a combination of genetic risk and environmental factors cause T1D, we still don’t know all the factors involved and how they lead to disease. In this research, Prof Barry will use cutting-edge genomic technologies to unravel the genetic risk for T1D, and understand more about the specific genes that are involved.
Using samples from the 1,500 mothers and babies enrolled in the ENDIA study, Prof Barry will perform genomic analysis on immune cells, which will allow researchers to link a person’s genetic risk of developing T1D to specific regions of the genome. This will help with building a world-first map of the connections between genetic risk regions for T1D and the immune system genes that they are associated with.
Researchers can then potentially target specific genes with interventions in clinical trials, moving towards an era of personalised medicine – where people with T1D can receive targeted treatments based on their own unique genetic makeup.
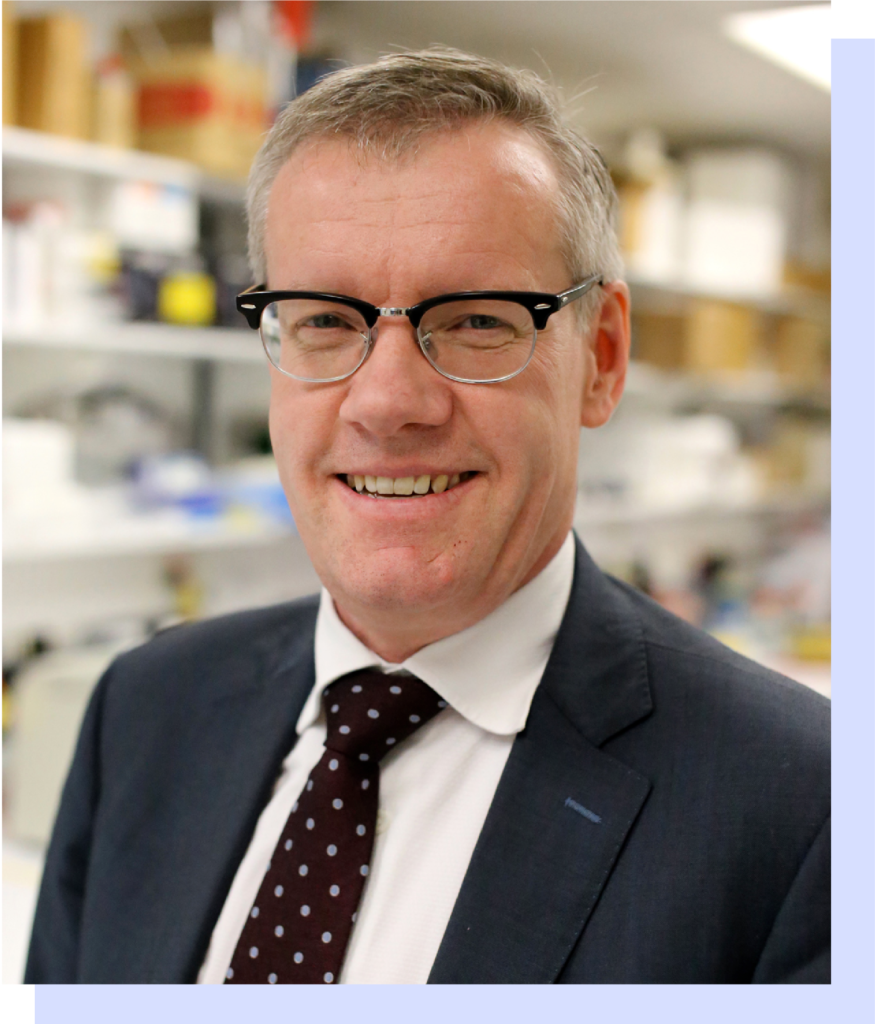
Prof Toby Coates, Royal Adelaide Hospital
A game changing new method of islet transplantation
Islet transplantation is a life-changing treatment for people with severe T1D. The current method involves transplanting islet cells into the liver, but this can be invasive, difficult to monitor, and requires a large number of cells for success.
Prof Coates has developed a new method of islet transplantation under the skin, using an artificial skin graft originally approved for use in burns patients. This graft provides the transplanted cells with their own blood supply, making them much more likely to survive after transplantation.
This highly innovative approach is now being trialled in people with type 1 diabetes for the first time. If successful, it could be a game changing new approach for islet transplantation – able to be performed under local anaesthesia, easy to monitor or remove, and significantly less expensive.
Prof Josephine Forbes, Mater Research and The University of Queensland
Using nanotechnology to prevent beta cell attack
Prof Forbes and her team have identified a promising new therapy, called soluble RAGE, that targets an important pathway in the development of T1D. In lab studies, soluble RAGE has been shown to slow the progression of early-stage T1D, but therapies of this type are difficult to administer effectively.
In this new project, Prof Forbes will investigate cutting edge drug delivery techniques using nanotechnology. Two different approaches will be tested: an oral treatment and a skin patch, both using tiny nanoparticles to deliver soluble RAGE more effectively into the body. and slow progression of T1D. If these delivery methods are successful, soluble RAGE could be tested in clinical trials as a potential new treatment for delaying the onset of type 1 diabetes.

A/Prof Shane Grey, Garvan Institute of Medical Research
Harnessing an inactivated virus to transport drugs directly to beta cells
One of the most exciting areas of T1D research is the discovery of therapies that can protect beta cells from immune system attack – or even regenerate them. However, researchers face the challenge of getting these therapies to where they are needed in the body.
A/Prof Grey, in collaboration with A/Prof Leszek Lisowski from the Children’s Medical Research Institute, is working on an innovative way around this problem. Viruses have evolved over millions of years to be able to efficiently invade specific cells, and A/Prof Lisowski has developed a technique to safely harness this ability and use it to deliver drugs.
In this new study, A/Prof Grey will use this delivery technology to transport the A20 gene, which his team previously discovered can protect islet cells from immune system attack. Once this gene has been delivered to beta cells, the cells will start producing their own copies of A20, potentially shielding them from the immune system.

A/Prof Stuart Mannering, St Vincent’s Institute of Medical Research
Investigating antibodies to unravel the causes of T1D
Before a person develops the physical symptoms of T1D, they have often developed markers of the disease – known as islet antibodies – within beta cells. However, the specific role of islet antibodies in the development of T1D is still unclear. A/Prof Mannering and his team believe that other components of the immune system, known as helper T cells, could work together with antibodies to ultimately cause T1D.
In this research, A/Prof Mannering will test this idea for the first time by investigating whether helper T cells recognise the specific part of islet antibodies that destroy beta cells. If true, it could dramatically change our understanding of how T1D develops. This could lead to innovations like new diagnostic tests, or therapies that can stop the T cell response and prevent T1D from developing.