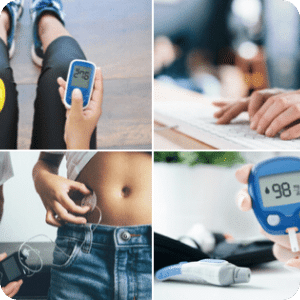
Type 1 diabetes guides & education
Find free books and resources to help you at every age and stage of life with T1D.

JDRF provides support and guidance for people with type 1 diabetes (T1D) at every step of their journey.
We’ve developed a variety of programs and resources, regardless of what age or stage you’re up to. Check them out and download your free resources below.
Type 1 diabetes: a guide for friends and loved ones
Do you know someone who has been diagnosed with type 1 diabetes (T1D)? Download our new guide to learn the basics of T1D, including how it’s managed, what people with T1D want you to know, and how you can help.
Learn more
If You’re Okay, They’re Okay: A guide for parents & carers
Our new free resource has been written especially for parents and carers of children and teens living with T1D. It offers valuable advice to help the whole family cope with life after a T1D diagnosis.
Learn more
Straight to the Point: A guide for adults living with T1D
This book is full of tips and resources to help you live a safer, easier and happier life with T1D as an adult. It addresses commons questions and concerns about living with T1D as an adult.
Learn moreTesting Times: A guide for teens living with T1D
This is the free must-have guide for teens and young adults living with type 1 diabetes. Get practical advice and tips on studying, managing stress, exercise, food and transitioning into adulthood while managing T1D.
Learn moreTeen Toolkit: A guide for parents of teens
Navigating the teenage years with T1D can be difficult. This guide is specifically for parents to help them with strategies to make their teenager’s journey a much more manageable experience.
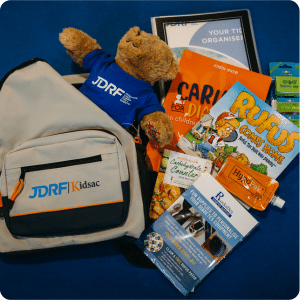
Learn moreKIDSAC: The pack for newly diagnosed kids and teens
JDRF’s KIDSAC pack aims to help support families in the difficult period following a T1D diagnosis. The free pack offers practical information, helpful products, and comfort to the child.
Learn moreVideos: exercise advice for people living with T1D
There is no doubt that exercise is good for you, but being more active may affect your blood glucose levels. To manage activity you need to understand a bit about how to move your body safely.
Learn morePodcast: The T1D Tune In
JDRF’s podcast, hosted by journalist Andrew Geoghegan, shares inspirational and interesting stories of adults living with type 1 diabetes. Listen to seasons 1 and 2 for free now.
Learn moreT1Directory
Our T1Directory is where we share all of the names of people, organisations and websites that make life with T1D a little easier.
Read the T1DirectoryRufus and his app
Learn about life with type 1 diabetes with Rufus. His app, available for Apple and Android, opens up a fun new world of education and play for your child with T1D.
Download the appHow to access mental health services with type 1 diabetes
Our official guide to accessing mental health services for people living with T1D. This resource was created in consultation with clinical psychologist Dr Rosalyn Taylor.
Read the mental health guideSnacking 101: An explainer for people living with T1D
The experts give us the low-down on all things snacking. The post includes tips & tricks for snacking from Dr Carmel Smart and Emma Fisher, paediatric diabetes dietitians at the John Hunter Children’s Hospital.
Read the snacking 101 guideAll about credentialled diabetes educators (CDE)
You might have already heard of, or seen a CDE, but you may not be aware of just how much in-depth specialist knowledge and skills they possess. Learn more about CDEs & how they can support you in this blog post.
Read about CDEsTurning an idea into a T1D breakthrough
Getting a new T1D treatment or device to market can take around 12 to 15 years. Learn how a research idea can become a breakthrough for someone with T1D.
Find out moreHow does a clinical trial work?
Before any new drug, device, or test can be made available to the public, researchers need to gather evidence that it is safe and effective for people to use in a clinical trial. Read this blog post to find out the steps involved in carrying out a clinical trial.
Learn more
I am interested in hearing more about…