Peter Larsen’s 61-year journey with type 1 diabetes

Meet Peter Larsen, a bright 86-year-old from Perth who has navigated the twists and turns of living with type 1 diabetes (T1D) for over 60 years. As a medical doctor, anatomy teacher, and pathologist, Peter learned to be resilient and adaptable while living with T1D, and has experienced an evolution of treatments during that time. Plus, he has also become an important advocate for better diabetes care in the community.
Peter’s wife of 59 years, Rosa (pictured above, with Peter), has been his partner through the ups and downs of his T1D journey. They have two children – a daughter living in Perth and a son in Toronto. Peter and Rosa’s son now also lives with T1D.
Spirit lamps and test tubes
Peter’s personal journey with T1D began at the age of 25, but diabetes was already a family affair.
“I was born into a diabetic sort of situation,” he says. Peter’s father, Arthur, a champion golfer, managed T1D with early insulin treatments.
“I remember the old spirit lamp – methylated spirits in a little glass lamp, and my dad would light the wick,” recalls Peter. Having put some Benedict’s solution and a couple of drops of urine in a test tube, he’d boil it up over the spirit lamp.
“And it was wonderful if it was sky blue. Sky blue meant there was no sugar in the urine. But more often than not, it was orange or brick red – and brick red was high. But, of course, testing of the urine in those days gave you a bit of information, but it was of very limited value and meant almost nothing.”
Peter’s mother, Freda, had type 2 diabetes, and his sister, Ida, developed T1D in her 50s. Peter’s own diagnosis came as he was starting his career as a doctor, adding another layer of complexity to his professional and personal life.
Peter’s father died when he was in his late 60s – a fate that Peter was told he was destined to emulate.
 Peter (right) with sister Ida (left) and mother Freda (centre)
Peter (right) with sister Ida (left) and mother Freda (centre)
TES-TAPE and home glucose monitoring
Peter says the process his father had to go through was cumbersome and mostly misleading, making effective diabetes management challenging. Home blood glucose monitoring was still many years away!
After Peter was diagnosed with T1D, he used TES-TAPE to test for glucose in his urine.
“This tear-off tape came in a little reel,” he says. “It was a big advantage because it was quick and easy to test with and being impregnated with an enzyme and it could actually test for glucose. Whereas early methods just tested for sugars of all sorts, this was specific for glucose.”
“But it was extremely unreliable to manage one’s sugar,” he says. “It couldn’t diagnose hypoglycaemia, for instance. All you could see was lots of glucose. And over the years I know that I was very poorly controlled.”
A giant step forward was the introduction of the first blood test strip, called Dextrostix, in 1965. It was a finger-prick test; a large drop of blood was placed on the strip, and after 60 seconds the blue colour was compared to a chart that indicated blood sugar level. It still wasn’t very accurate.
The next advancement was the development of a Reflectance Meter, which could read the Dextrostix test-strip more accurately. This was the forerunner of the modern blood glucose monitor.
But these products still weren’t meant for self-testing; the meter was very expensive, as were the strips.
“Self-monitoring blood glucose at home came about slowly. I managed to get around the expense by cutting the re-agent pad on the Dextrostix strip into 8 tiny squares, each of which I mounted on a thin strip of card. I then made my own colour chart, which was far more accurate than the chart on the Dextrostix bottle! Now I could check my sugar umpteen times a day as needed, and that stood me in good stead for a few years,” Peter says.
The next important leap in diabetes care was in the 1980s, when home glucose monitoring became established and widespread. Re-agent strips were redesigned so smaller amounts of blood were needed. By the end of the 1980s, enzyme electrode strips were being used in the newly developed and highly portable biosensor electrode metres, becoming more and more affordable.
“Home blood glucose monitoring was a very, very big step,” Peter recalls.
Self-monitoring meant people with T1D could measure their blood glucose levels by themselves for the first time – and then make their own treatment decisions based on those values.
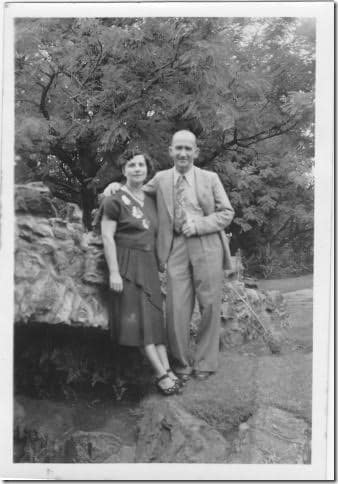 Peter’s parents, Freda and Arthur
Peter’s parents, Freda and Arthur
Insulin pumps and continuous glucose monitors
In the early 2000s, insulin pumps and continuous glucose monitors (CGMs) revolutionised the way T1D was treated in Australia and around the world, because for the first time, people with T1D could see their blood glucose levels in real time, and use the pump to deliver insulin as needed to manage blood glucose levels with little effort.
Peter started using a Tandem t:slim X2 pump about four years ago, in his early 80s, which he says has been “totally liberating and life changing!”
“I was very late in getting the pump actually,” Peter explains. He says he thought the cost would be prohibitive, then learnt his insurance would cover the entire cost.
Insulin pumps cost $7000 to $10,000 to purchase outright, but the cost is covered by some private health funds.
With the pump providing a more consistent and controlled delivery of insulin, Peter found not being burdened with multiple daily injections a great relief. But even more transformative has been the use of a continuous glucose monitor (CGM).
“Continuous glucose monitoring is the ultimate,” Peter says.
For Peter, the CGM has been life-changing, helping him avoid the dangerous highs and lows that come with diabetes.
“This CGM, it’s so important for diabetes,” he says. “It’s one of the biggest breakthroughs there’s been in diabetes, apart from insulin and other things like that. It’s a huge, huge breakthrough.”
Treating the next generation
It was only four or five years ago that Peter’s son, also called Peter (known as Peter George or PG to his family) was diagnosed with T1D.
“Rosa and I were naturally upset when our son was diagnosed, but it was picked up on a routine check-up and he was otherwise very fit, so we just accepted ‘it is what it is,’ and hoped that he would manage well.
“He continued to enjoy his long-distance running which was very beneficial with the condition, but he would have to watch his beers which he had also enjoyed!”
Peter says both his son and his sister had similar experiences when they were first diagnosed with T1D.
“Both were under the care of GPs who diagnosed and treated them as type 2 for a long time before eventually being referring them to a specialist physician or endocrinologist,” he says.
“I have an idea this is unfortunately not an unusual scenario, which could – and should – have been avoided. My son was on Metformin [tablets] for two or three years… After his referral to an endocrinologist he was put on multiple daily injections, and has only been on a pump for a couple of weeks. He is very happy with it.”

Peter’s son, PG, and family
Advocating for better T1D care
Peter’s advocacy also played a role in making CGMs more accessible to others in the community. “I wrote a couple of letters to members of parliament, arguing for a subsidy, and put a lot of effort into it,” he says.
“It took an awful lot for us to persuade them because they said, ‘Oh, okay, you can have it, as long as you’ve been admitted to hospital in a diabetic coma, then we’ll help you’,” Peter recalls.
“I had to really put across a very clever argument,” he says with a sly smile. “I said, I’m sorry, but I can’t oblige you by going into a coma.”
Peter’s efforts, along with the #AccessForAll campaign from members of the Diabetes Alliance, including JDRF, led to government subsidies for CGMs, making this life-saving technology available to more people with diabetes.
From glass syringes and unreliable urine tests to modern insulin pumps and CGMs, the progress Peter has seen has been remarkable.
“I’ve lived through the whole story virtually of diabetes,” he says.
To those who are just learning to live with T1D now, Peter says it’s important to take care of your overall health and to eat well.
“There’s no such thing as a diabetic diet, only a prudent diet for everyone,” he says. And he should know; as he points out, “I’ve had diabetes for just over 60 years now – longer than they said I would!”
Read more